Fentanyl addiction kills more Americans than any other drug, claiming over 70,000 lives annually. The synthetic opioid’s extreme potency makes withdrawal dangerous without medical supervision.
Searching for “fentanyl detox near me” can feel overwhelming when you need help immediately. We at Surf City Detox understand that finding the right program can mean the difference between life and death.
Professional medical detox provides the safety and support needed to survive fentanyl withdrawal and begin recovery.
Why Fentanyl Detox Requires Professional Medical Care
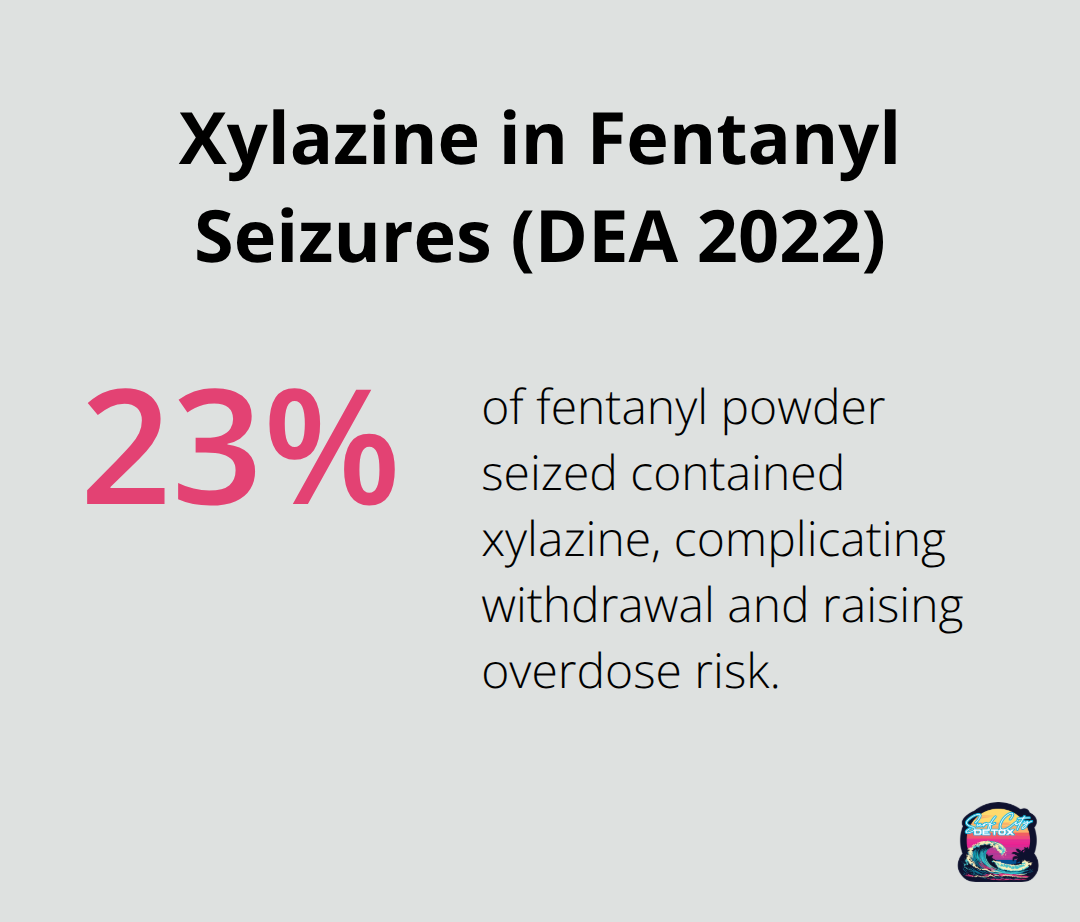
Fentanyl is a potent synthetic opioid drug approved by the Food and Drug Administration for use as an analgesic and anesthetic, which makes withdrawal symptoms severe and potentially fatal without medical intervention. The Drug Enforcement Administration reports that approximately 23% of fentanyl powder seized in 2022 contained xylazine, a veterinary sedative that complicates withdrawal and increases overdose risks.
Medical Complications Strike Without Warning
Medical complications during fentanyl withdrawal include seizures, severe dehydration, cardiac arrhythmias, and respiratory depression that can occur within hours of the last use. Temperature regulation becomes unstable, blood pressure fluctuates dangerously, and psychological symptoms like severe anxiety and suicidal thoughts peak within 48-72 hours. These complications develop rapidly and require immediate medical response to prevent death.
Professional Monitoring Saves Lives
Professional detox facilities provide continuous vital sign monitoring, IV fluid management, and immediate access to emergency medications that prevent withdrawal-related deaths. Benzodiazepines like lorazepam control seizures, while clonidine manages blood pressure spikes and reduces anxiety. The SAMHSA Advisory emphasizes that individuals with history of severe withdrawal problems require 24/7 medical supervision rather than social detox settings (not basic outpatient care).
Home Detox Attempts Create Deadly Risks
Home detox attempts fail because fentanyl withdrawal symptoms intensify rapidly and become medically dangerous without professional intervention. Dehydration from vomiting and diarrhea can cause kidney failure, while uncontrolled anxiety often leads to panic attacks that mimic heart attacks. Most people cannot distinguish between normal withdrawal discomfort and medical emergencies, which leads to delayed treatment that can prove fatal. Studies show that attempting fentanyl detox alone results in high relapse rates, primarily because the physical agony becomes unbearable without proper medication management.
The next step involves understanding what specific features and qualifications make a detox program truly safe and effective for fentanyl recovery.
How Do You Choose the Right Fentanyl Detox Program
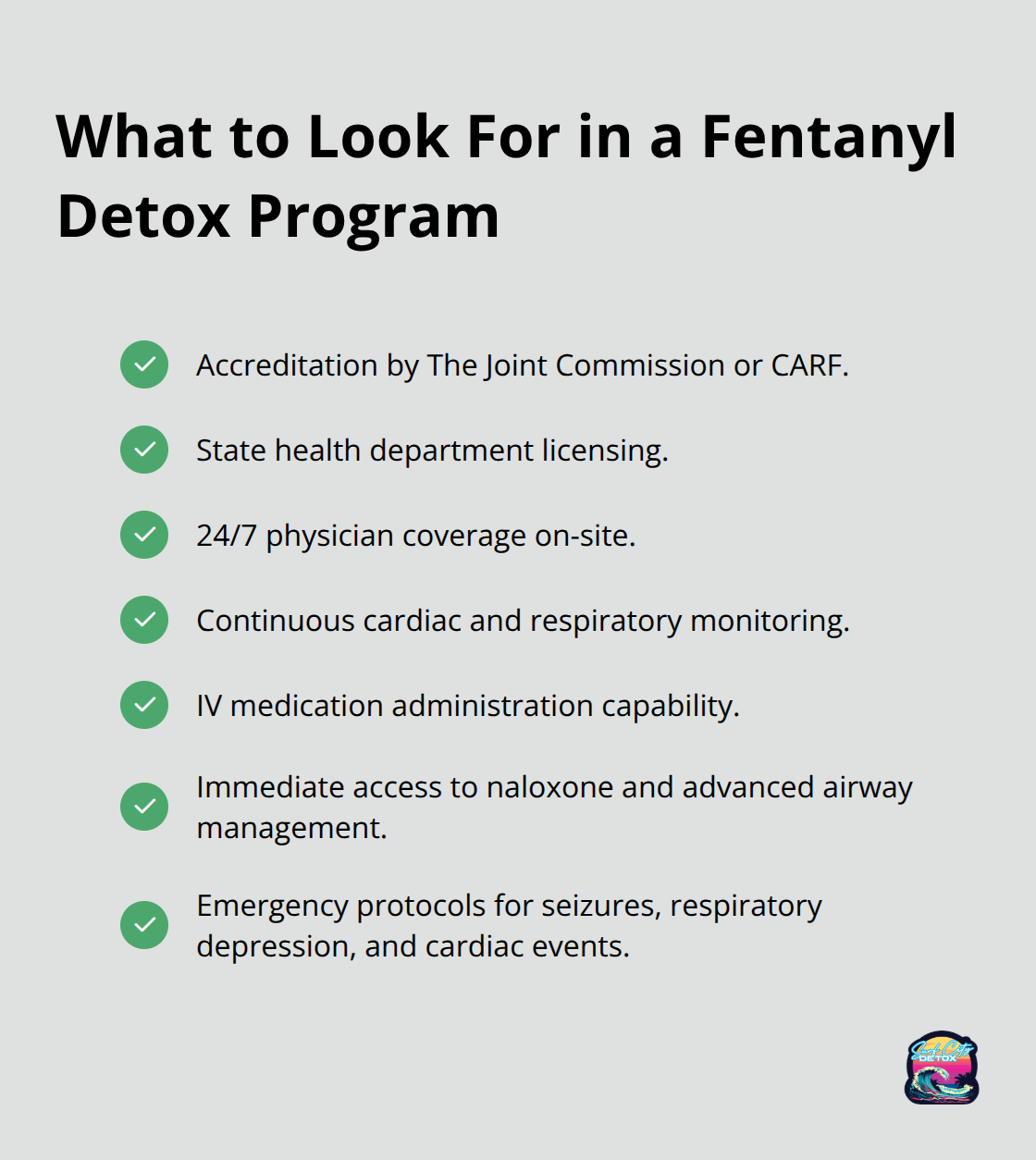
Fentanyl detox programs require specific medical capabilities that separate life-saving facilities from inadequate treatment centers. The Joint Commission accreditation and state licensing from health departments represent minimum safety standards, but fentanyl withdrawal demands specialized protocols beyond basic requirements. Quality programs provide continuous cardiac monitoring, IV medication administration, and immediate access to emergency interventions like naloxone and advanced airway management. The facility must maintain physician coverage around the clock, not just nursing staff, because fentanyl withdrawal complications require immediate medical decisions that nurses cannot legally make.
Staff Expertise Determines Survival Rates
Medical staff must demonstrate specific training in opioid withdrawal management through certifications from organizations like the American Society of Addiction Medicine or completion of buprenorphine prescribing courses. Ask about nurse-to-patient ratios during peak withdrawal periods (which should never exceed 1:4 for fentanyl patients). The medical director should hold board certification in addiction medicine or internal medicine with documented experience treating synthetic opioid withdrawal. Programs that use general medical staff without addiction specialization create dangerous gaps in care that lead to preventable complications and treatment failures.
Medication Protocols Save Lives During Crisis
Effective programs utilize FDA-approved medications including buprenorphine, methadone, and naltrexone for opioid use disorder management, with immediate access to comfort medications like clonidine for blood pressure control and ondansetron for severe nausea. The facility should maintain emergency protocols for respiratory depression, seizures, and cardiac events that occur during fentanyl withdrawal. Programs that rely primarily on non-medical approaches or limit medication access create unnecessary suffering and increase dropout rates. SAMHSA guidelines emphasize that medication-assisted treatment can be used to treat substance use disorders and sustain recovery.
Accreditation Standards Protect Patient Safety
Look for facilities accredited by The Joint Commission or CARF (Commission on Accreditation of Rehabilitation Facilities), which require rigorous safety protocols and regular inspections. State licensing from health departments provides basic oversight, but national accreditation demonstrates commitment to excellence in patient care. These organizations mandate specific staff-to-patient ratios, emergency response procedures, and quality improvement measures that protect vulnerable patients during withdrawal.
Facilities without proper accreditation may lack essential safety measures that prevent medical emergencies from becoming fatal complications.
The medical detox process itself follows specific stages and timelines that patients and families should understand before treatment begins (which helps set realistic expectations for the recovery journey ahead). Comprehensive programs include medically supervised detox, residential treatment, and dual diagnosis care to address co-occurring mental health conditions. Following detox, aftercare programs support long-term recovery with ongoing guidance and relapse prevention strategies.
What Happens During Fentanyl Medical Detox
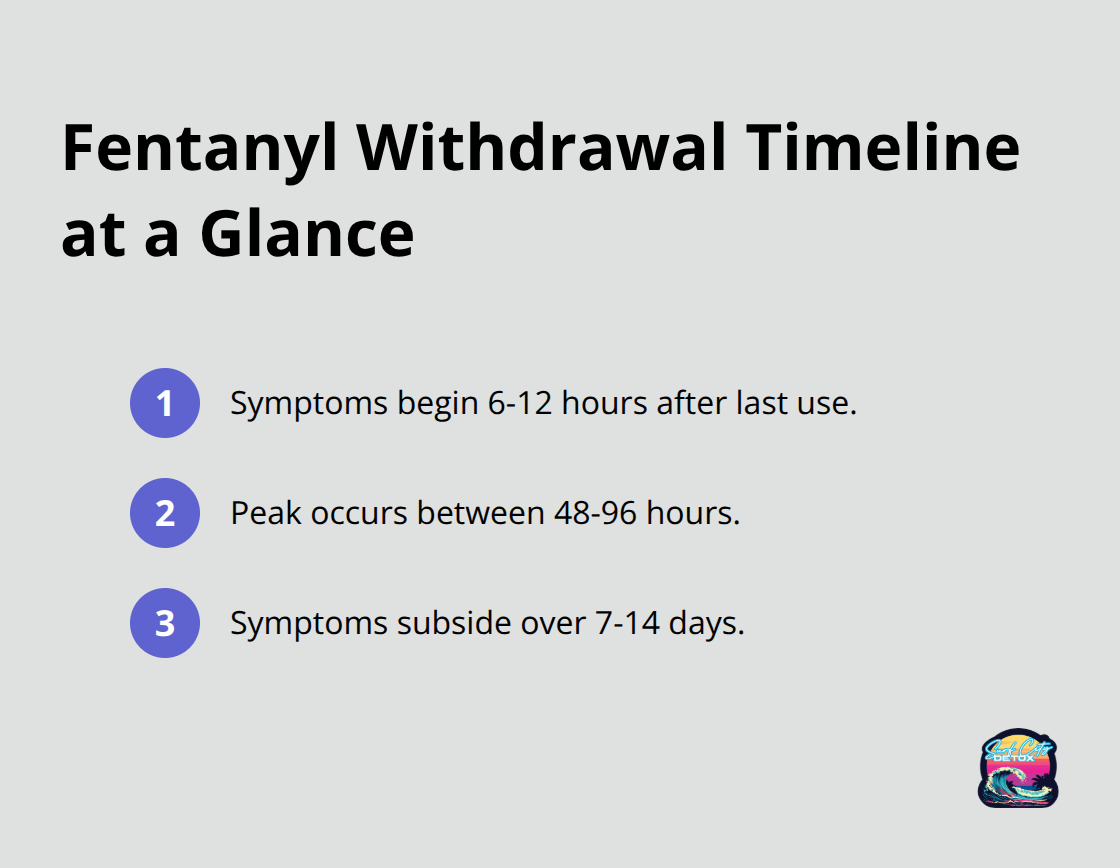
Fentanyl withdrawal follows a predictable timeline that medical professionals use to anticipate and manage complications before they become life-threatening. Symptoms typically begin 6-12 hours after the last use, peak between 48-96 hours, and gradually subside over 7-14 days. The Drug Enforcement Administration data shows that fentanyl creates rapid onset withdrawal that intensifies faster than heroin or prescription opioids.
Physical Symptoms Require Immediate Medical Response
Physical symptoms include severe muscle aches, nausea, vomiting, diarrhea, and temperature dysregulation that can become medically dangerous within hours. Psychological symptoms like anxiety, depression, and intense cravings can persist for weeks without proper medical management. Blood pressure spikes occur unpredictably, while dehydration from persistent vomiting creates kidney stress that requires IV fluid replacement.
Medical Protocols Control Dangerous Symptoms
Medical teams utilize FDA-approved medications including buprenorphine for opioid replacement therapy, which helps manage withdrawal symptoms during medical detox. Clonidine controls blood pressure spikes and reduces anxiety, while ondansetron prevents dangerous dehydration from persistent vomiting. Comfort medications like gabapentin address nerve pain and sleep disturbances that can last beyond acute withdrawal.
Professional Monitoring Prevents Fatal Complications
The key advantage of professional detox lies in immediate medication adjustments based on real-time symptom assessment rather than fixed protocols that ignore individual variations in withdrawal severity. Medical staff monitor vital signs every four hours during peak withdrawal periods (days 2-4) and adjust medications based on symptom severity scores. Emergency protocols activate when patients develop seizures, cardiac arrhythmias, or respiratory depression that can occur without warning.
Treatment Transitions Begin During Detox
Medical detox represents only the first phase of fentanyl addiction recovery, typically lasting 5-10 days depending on individual factors like duration of use and overall health status. Successful programs begin discharge planning on day one, connecting patients with residential treatment, intensive outpatient programs, or medication-assisted treatment continuation. Studies indicate that individuals who transition directly from detox to structured treatment programs achieve higher long-term sobriety rates than those who attempt recovery without ongoing support. The medical team evaluates each patient’s readiness for the next treatment level using standardized assessments that consider physical stability, mental health status, and social support systems available upon discharge.
Final Thoughts
Fentanyl addiction demands immediate professional intervention because every day without treatment increases fatal overdose risk. The synthetic opioid’s extreme potency makes self-detox attempts dangerous and often unsuccessful, while medical supervision provides the safety net needed to survive withdrawal and begin recovery. Professional help saves lives through continuous monitoring, emergency medical response, and evidence-based medications that control dangerous withdrawal symptoms.
Medical teams prevent complications like seizures, cardiac events, and respiratory depression that can occur without warning during fentanyl withdrawal. When you search for “fentanyl detox near me,” prioritize facilities with Joint Commission accreditation, 24/7 physician coverage, and specialized opioid withdrawal protocols. Quality programs provide immediate access to FDA-approved medications, emergency interventions, and seamless transitions to ongoing treatment.
We at Surf City Detox provide medically supervised detoxification with clinical monitoring in Huntington Beach, California. Our approach combines medical detox, residential treatment, and dual diagnosis care under one roof (addressing both addiction and underlying mental health conditions that fuel substance use). Recovery begins with a single phone call to qualified professionals who understand fentanyl addiction’s complexity and provide the medical expertise needed to survive withdrawal safely.



